
So, I actually didn’t know a thing about my pelvic floor until after I had my daughter. But I wish I did!
It’s a part of the body you really never think about when everything is working well.
Turns out though, the pelvic floor and deep core muscles are the muscles most impacted by pregnancy and delivery. After pregnancy, those muscles have a tendency to misbehave.
Fun fact:
Your pelvic floor stretches 3.5 times it’s resting length during labor (if you delivery vaginally)!
Before that, it spends a lot of months supporting a heck of a lot of extra weight.
Right after you have a baby, there’s a pretty good chance that something isn’t going to be working quite like you remember (leaks, pressure-y feelings, stuff bulging).
But, no fear mongering here!
There are a lot of (very effective) tools and resources available to support you through the rehab and recovery of your pelvic floor after birth. As is the case with so many things, the more you know, the more proactive you can be.
Here’s the stuff I wish I knew:
The Anatomy And Function Of Your Pelvic Floor Muscles
Your pelvic floor is a set of muscles and connective tissue that sit inside of your pelvis. It stretches from tailbone to pubic bone, and sitz bone to sitz bone. It’s roughly the size of an 8.5″ x 11″ piece of paper!

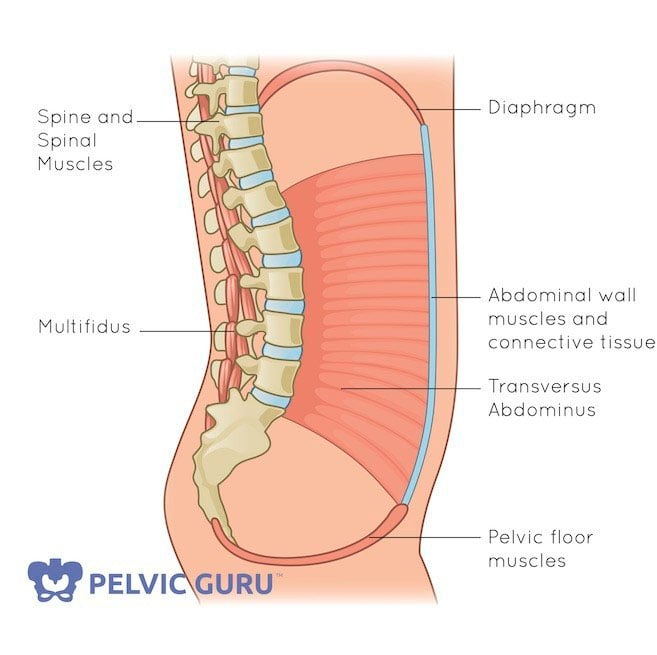
These muscles form a canister, with the diaphragm on top and the pelvic floor on the bottom- the transverse abdominals and multifidus form the walls. As the bottom of the canister, the pelvic floor also provides support for all of your organs that lie above it.
Your core “canister” is a pressure system that responds to your breathing cycle. When you inhale, your diaphragm should contract downwards, creating pressure in your abdomen. Your pelvic floor responds to increased pressure by lengthening downwards. As you exhale, your diaphragm contracts upwards and your pelvic floor recoils.
Throughout a diaphragmatic breath cycle, your pelvic floor goes through a full range of motion that contributes to its optimal function.

In addition to supporting your organs and contributing to your overall stability, your pelvic floor also helps maintain continence (control of your bladder and bowel) and contributes to sexual sensation.
Your pelvic floor is somewhat unique in that it functions under voluntary and involuntary control. Without you thinking about it, your pelvic floor does all the things we just talked about. But, you can also consciously squeeze or clench these muscles. The act of squeezing the pelvic floor muscles is often called a “kegel”.
Pelvic Floor Dysfunction
The female pelvic floor has three openings (the urethra, the vagina and the anus) and thus there are three ways to squeeze the pelvic floor. Relative the male pelvic floor, the female pelvic floor has an extra opening (no big surprises here, I hope!). This extra opening is what makes the female pelvic floor a bit more susceptible to pelvic floor conditions like incontinence and pelvic organ prolapse.
In an optimally functioning pelvic floor, the muscles aren’t too tight or too lax. They’re just right. But for many people, these muscles tend towards one extreme or the other.
Muscles can become “tight” (high-tone or hypertonic) due to overtraining, chronic stress and anxiety, physical trauma or abuse. Muscles may be too “loose” as a result of a variety of factors including pregnancy and aging. If the pelvic floor muscles are too tight or too lax, they will not contract or relax (or support!) in an optimal way. In this case, they are often labelled “dysfunctional”.
The symptoms of pelvic floor dysfunction, whether due to a too tight or too loose pelvic floor, can look outwardly similar. For example, both can cause incontinence (leaking), pelvic pain or discomfort and sexual dysfunction. The treatments for either extreme are different, making it really important that if you do experience any unusual pelvic symptoms you don’t self-treat with a million Kegels.
If you think you need to do a million kegels, it’s time to reach out for professional guidance.
The most appropriate medical professionals to consult with for pelvic floor disorders are pelvic floor physical therapists (sometimes called Women’s Health physical therapists). On my resource page, I link to several websites that can help you track down a pelvic health physical therapist.
Pelvic Floor Dysfunction In Pregnancy and Postpartum
During pregnancy and postpartum, symptoms of pelvic floor dysfunction are very common. If you experience leaking (of anything), pelvic discomfort, painful sex, or feelings of pressure through your perineum or vagina (perhaps like a tampon falling out), consult a pelvic floor therapist. If you want to be proactive about your pelvic health during your pregnancy, I advise booking a session with one.
During a prenatal pelvic floor physical therapy appointment, your PT can establish your pelvic health baseline, work with you to ensure your pelvic muscles and ligaments are in good shape for labor and delivery, teach you things like perineal massage and even help you determine which labor positions might work best for your body. I also strongly encourage everyone to schedule a 6 week postpartum check-in with a pelvic health physical therapist regardless of whether or not they’ve ever had a problem or not. These professionals are uniquely qualified to evaluate the health and function of your pelvic floor and assess your readiness to return to exercise. If you are an athlete or itching to return to your workouts, don’t skip this step!
Are Kegels The Answer?? Maybe Not!
A side note on kegels: kegels are isolated pelvic floor muscle contractions. However, the pelvic floor isn’t designed to work in isolation.
The pelvic muscles work as part of a coordinated team and this team works best when the function of all its members is balanced. By overtraining one member, by over-kegel-ing for example, you can throw off that balance.
As a personal trainer and a birth doula, I firmly believe it is outside of my scope to assign or prescribe kegels.
Why?
1) Many people kegel incorrectly.
Many people actually bulge their pelvic floor muscles instead of contracting them. Consistently performing excessive numbers of reps of an incorrect kegel (like the 100s I see recommended on some pregnancy and postpartum sites!) can potentially lead to problems.
Pelvic physical therapists are the only professionals who are qualified to assess the quality and accuracy of your kegel. While I can ask questions about what you’re feeling and offer a variety of cueing, ultimately, it’s outside of my scope of practice to assess your kegel. Since I can’t assess your kegel, I don’t assign you kegels.
2) Even if you can Kegel properly, you might not need to.
Your muscles might not be weak. They might be tight or they might just be out of sync with their team. In both of these scenarios, continuing to kegel many cause further problems.
A kegel is something that should be prescribed by a pelvic floor physical therapist who has done a thorough assessment of your body and biomechanics.

Personal Training For Your Core And Pelvic Floor
Since we’re leaving kegel assignment to physical therapists, where does that leave a core and pelvic floor-informed personal trainer? While we can’t assign kegels, we can help you to:
- Connect with your pelvic floor and inner core through a variety of breathing strategies
- Breathe in a manner that is supportive to your exercise and activities of daily living
- Manage your symptoms of pelvic floor dysfunction
- Transition you from rehab exercises to higher level activities and sports
We can complement your physical therapy program and help you move beyond it. A good pre/postnatal trainer will craft exercise programs with your specific pelvic health considerations in mind and will be more than happy to collaborate with your physical therapist if that is helpful.
In my coaching practice, I teach people how to contract their pelvic floor in coordination with the rest of their inner core using a breathing strategy called the Connection Breath. The Connection Breath trains the coordination and optimal function of the core and pelvic floor by integrating kegels with diaphragmatic breathing. It is practiced just enough to automate the coordination of and support the reflexive function of the core, but is not meant to strengthen the pelvic floor in isolation.
A Little Maintenance Goes A Long Way
Most people aren’t going to get to know their pelvic floor until it acts out. But that doesn’t need to be the case.
With just a bit of care and attention, you can keep your pelvic floor functioning optimally throughout your pregnancy and postpartum.
Good alignment, breathing and movement strategies can go a long way towards fending off or managing leaking and pelvic floor discomfort and they’re part of good long-term pelvic health habits.
For more guidance, check out the resources in the “Take Action” section below!
Take Action!
- Are you pelvic floor-curious? Download a FREE copy of the No B.S. Guide to a Stronger, Drier Pregnancy and Postpartum. Consider it a user manual for your pelvic floor! This guide will teach you good habits around body alignment, breathing and managing effort during exercise that will keep your pelvic floor in tip top shape.
- If you’re experiencing pelvic pain, discomfort or leaking during exercise or functional movements of daily life, consider a one-on-one consultation to get individualized advice.
- Leave a comment below! Tell me, what inspired your interest in your pelvic floor muscles- Are you pregnant? Postpartum? Or trying to troubleshoot some pesky symptom?
Take a deep dive into HOW to dial in your alignment, breathing and movement strategies:
Download a FREE copy of The No B.S. Guide to a Stronger, Drier Pregnancy and Postpartum.

My mission is to make sure that having a baby is not a reason why you can’t do all the things.
Contact me with questions about exercise or pelvic health pertaining to pregnancy or postpartum. I work with people online and in-person (Seattle-area, Bellevue, Redmond, Kirkland) to develop personalized pregnancy and postpartum exercise plans.
Certified Prenatal & Postnatal Coach, Pregnancy & Postpartum Athleticism Coach and Postnatal Fitnesses Specialist.






