
Baby Max is 3 weeks old today. So, I am 3 weeks postpartum! Up until this week, my movement has consisted entirely of easy walking and gentle core and pelvic floor exercises. This movement has felt great and I’m feeling ready for a little bit more. This next week, I will add in some gentle movements, no more difficult than movements of daily living (for example, body weight squats, heel slides and scapular retractions). But, before I start, I want to know what my abdominal muscles are doing. In this post,
In this post, I’m going to walk you through the steps I used to assess the separation between my abdominal muscles (–> self-assessment for Diastasis Recti).
The Reality of Diastasis Recti
According to research, up to 100% of women have a Diastasis Recti (DR; a clinically significant separation of the rectus abdominus muscles, a.k.a. six-pack muscles) by the end of the third trimester.
The separation of the abdominal muscles is actually a thinning and stretching of the linea alba and the connective tissue encasing the abdominal muscles; it is the body’s way of making space for a growing baby.
The most intensive spontaneous healing occurs during the first 8 weeks. Nothing observed earlier than 6-8 weeks postpartum necessarily has much value as a diagnosis or a major cause for concern. In fact, there may not be a ton of value in assessing DR until at least 6 weeks, because any separation prior to that is still pretty normal. But I like data, so I’m checking myself.
3 steps to Diastasis Recti self-assessment
1. Check out the tension along your abdominal midline.
Lie on your back, knees bent. Use your fingers to press into the abdominal wall along the linea alba (centerline of 6-pack muscles) from sternum to pubic bone. Observe whether or not there is variability in the tension along the linea alba.
2: Assess your abdominal separation (diastasis).
Place three fingers across the midline just above the belly button. Tuck your chin and lift the head (not the shoulders!) just to the point where the abdominal muscles activate (not a big crunch). You should feel the edges of the rectus muscles hug your fingers, although you might need to adjust the number of fingers (or hands) you are using to span the gap. Assess the gap at the belly button, at three fingers height above the belly button, and at three fingers distance below the belly button. Take note of how squishy or taut the tissue is. How many knuckles deep do your fingers go?
3. Reassess your separation along with an exhale breath.
Reassess the same three spots (at, above and below belly button) while you exhale to engage your abdominal muscles. To do this, exhale through pursed lips, like you are blowing out birthday candles. As you feel your muscles hug your fingers, make note of the separation between your muscles and the squishiness of the tissue.
Bonus points: Reassess your separation along with a Connection Breath.
Reassess the same three spots as above, while performing a connection breath (a pursed lip exhale with a pelvic floor contraction.
If you can do a pelvic floor contraction at the same time that you exhale, do it If you can’t, just focus on the strong, forced exhale (step #3). Hopefully, you feel your core muscles contract in response to your exhale breath. Does the width or tension in the Linea Alba change in response to core activation?
Take note of this data. The numbers are not good or bad, but they will given you a baseline as you figure out how things are changing over the next few weeks. Avoid the temptation to check your DR every week. There’s too much noise in the data and changes to the tissue take time. I suggest no more frequently than every 3 weeks.
The results of my self-assessment
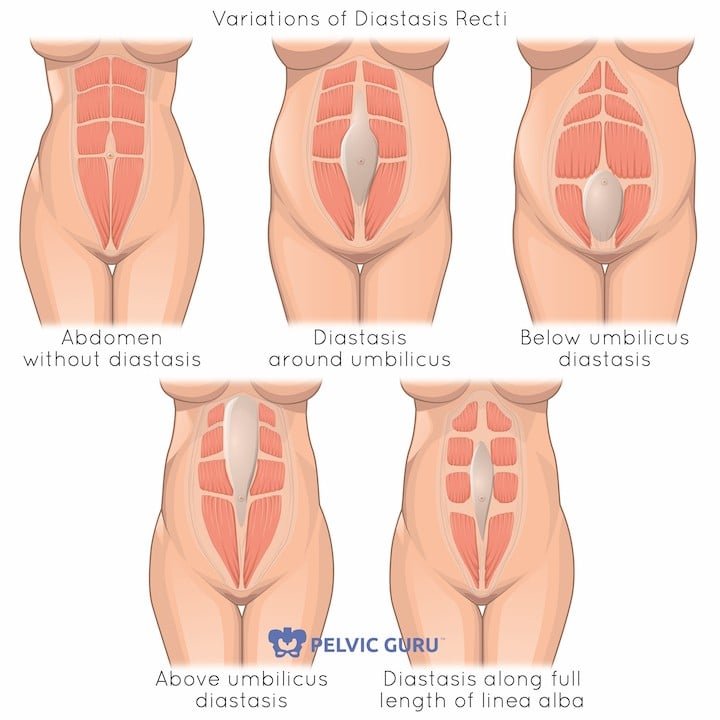
When I felt my linea alba without a head lift, I felt the least tension right around my belly button. When I lifted my head, I felt a three finger gap at the belly button. I was able to sink my fingers in up to about my first knuckle. Three fingers above my belly button, the gap was about two finger widths with good tension and three fingers below my belly button, the gap was one finger width with good tension.When I add in a connection breath, the gap at my belly button reduces to two fingers, although I don’t have much improvement in tension. The gap reduces to one finger width below my sternum and less than one finger width above my pubic bone. All of these observations are consistent with my abdominal separation being widest right around my belly button. The shape of the abdominal separation can vary widely individual to individual (see the image below), and this information can be useful as you’re rehabbing so you know where to focus your abdominal work.
A three finger-wide diastasis at 3 weeks postpartum is certainly nothing to worry about. Diastasis Recti is now defined not only by width but by tension as well.
Many research studies and clinicians use a 2 cm (roughly 2 finger-width) cut-off to diagnose DR, but the ability to generate tension in the tissue is even more important and more diagnostic. So, don’t worry about a separation of less than 2 cm if you are generating good tension with a core and pelvic floor contraction. Similarly, you likely don’t need to worry about a somewhat larger gap if you are able to generate good tension in it when you activate your core and pelvic floor.
If you are concerned at all about what you are feeling, book an appointment with a pelvic floor physical therapist (a good idea anyway) and work with a qualified postnatal fitness specialist to assess your situation and work towards rehab and retraining.
Learn the foundational strategies for healing Diastasis Recti. Download a FREE copy of
The No B.S. Guide to a Stronger, Drier Pregnancy and Postpartum.👇🏽👇🏽

My mission is to make sure that having a baby is not a reason why you can’t do all the things.
Contact me with questions about exercise or pelvic health pertaining to pregnancy or postpartum. I work with people online and in-person (Seattle-area, Bellevue, Redmond, Kirkland) to develop personalized pregnancy and postpartum exercise plans.
Certified Prenatal & Postnatal Coach, Pregnancy & Postpartum Athleticism Coach and Postnatal Fitnesses Specialist.






